Sign up for Devex CheckUp
The must-read weekly newsletter for exclusive global health news and insider insights.
When the World Health Organization designated 2021 as the International Year of Health and Care Workers, it also urged that the world’s health care workers be prioritized for vaccination against COVID-19 in the first 100 days of 2021.
While countries like the United States have vaccinated 63% of their adults, others have not even been able to vaccinate populations at high risk of infection, including those on the front lines. Currently, only 1.86% of the African population has been reached with a first dose.
Despite WHO’s recommendations, unequal access to vaccines is stalling progress. “The world came together and agreed that health care providers should be the first ones to get vaccinated globally, plus the people at risk, before [starting to] vaccinate people who are not at risk in the developed world. And they didn’t respect that commitment,” Agnes Binagwaho, vice-chancellor of the University of Global Health Equity and Rwanda’s former health minister, told Devex.
At least 17,000 health workers have died from COVID-19 over the last year, according to an analysis by Amnesty International, Public Services International, and UNI Global Union which have all called for urgent action to speed up the vaccination of millions of front-line health workers who continue to risk their lives in the response. According to a 2020 study in the U.K., health care workers are seven times as likely to have severe COVID-19 as other workers.
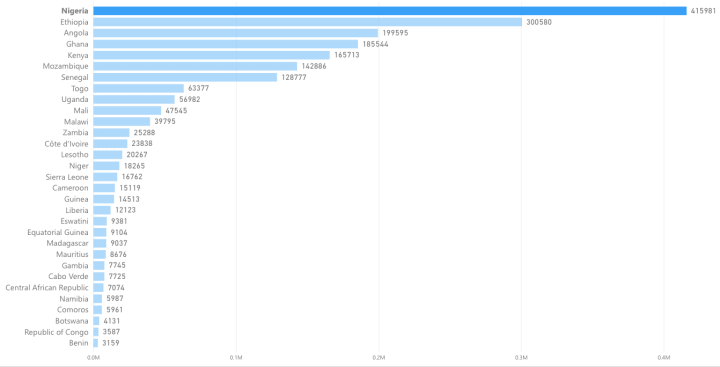
WHO relies on reporting from countries to track their vaccination efforts — including for priority groups — but many face challenges in collating and reporting data, particularly from outside capital cities. So far, 34 African countries have reported administering almost 2 million doses to health care workers, according to available data published by WHO.
WHO is working to better understand the reasons for varying uptake of vaccines by health care workers, said Dr. Phionah Atuhebwe, the regional new vaccines introduction medical officer, who is coordinating the WHO Africa COVID-19 Vaccine Readiness and Equitable Delivery Taskforce.
“It remains a priority not only because health workers remain at highest risk of COVID-19, but also research shows that health workers strongly influence others to take the vaccine,” she wrote in an email to Devex.
Beyond prioritizing
In theory, countries are following recommendations and prioritizing the vaccination of health care workers in their national deployment and vaccination plans — the operational plans to implement and monitor the COVID-19 vaccination rollout that they must submit to the international COVAX initiative, said Alex de Jonquieres, director of health systems and immunization strengthening at Gavi, the Vaccine Alliance.
“In a pandemic like this, systems can start getting overwhelmed so you need to have protected the health care workers as the front-line so that they can keep the systems going.”
— Dr. Willis Akhwale, chairman of the national task force on vaccination, Kenya
But the inoculation of health care workers depends on the overall success of countries’ vaccination campaigns. “Because of the supply constraints and particularly because of the situation in India, supply is coming through more slowly than we had anticipated,” said de Jonquieres.
With India battling a large second wave of COVID-19, many of the low-income countries that had signed up to COVAX are facing delays in receiving their Serum Institute of India-manufactured doses due to the increased demand for COVID-19 vaccines in India.
Fixing the supply problem overall, being ambitious in dose sharing from donor governments, and ramping up capacity by manufacturers are going to be critical, he added. Rwanda, Kenya, South Africa, and Nigeria have all reported vaccine shortages that will impact the progress of inoculating their health care workers.
“In a pandemic like this systems can start getting overwhelmed so you need to have protected the health care workers as the front-line so that they can keep the systems going, [so that] they are able to attend to any surges that may occur,” said Dr. Willis Akhwale, chairman of the national task force on vaccination in Kenya.
Get development’s most important headlines in your inbox every day.
Thanks for subscribing!
Reaching health care workers
Only a small number of countries did actually budget for COVID-19 vaccine delivery in their health budgets this year. For example, analysis looking at models of delivery costs have shown that for low-income countries, reaching 20% of their population will require at least a 20% increase in their overall health budget, said de Jonquieres.
“For health care workers in urban centers, in particularly in capital cities, it’s less of a problem because it’s actually quite easy to deliver their vaccines … but reaching those out in the periphery is challenging, because you need operational cost either to go out to them or to bring them to where the vaccine is available,” he said, adding that Gavi is making bridge funding available to countries where there is a critical need and where that lack of operational budget risks wasting vaccines that can’t be administered before they expire.
Data and planning are behind Kenya and Rwanda’s success stories
Smart data management key to successful vaccine rollouts
Some countries are struggling to roll out the COVID-19 vaccines they have, whereas Rwanda rapidly administered the doses it received. Much of this was due to smart data management.
In Kenya, the ministry of health asked each of the counties to supply the number of health care workers — both in the public and private sector — within their jurisdictions. Coupled with already existing databases, they were able to identify the number of formal health care workers and other staff working within health institutions who needed to be prioritized for the vaccine, said Akhwale.
However, accurate data on community health care workers is more difficult to access. “We estimated there could be anywhere around about 200,000. Now, these ones are so much in the community and we’ve not tracked them separately, yet. Part of the reason is their definition and available records vary so much between one county to another,” he added.
According to Binagwaho, it’s a matter of planning and self-organizing. In Rwanda, community health care workers normally meet in the health center they report to once per month — there are about 500 in the country, and the centers in turn report to a district hospital. “So the community health workers went to get the vaccine where they used to report,” she said.
When Rwanda received 240,000 doses of the AstraZeneca vaccines through COVAX on March 3, the shots were quickly distributed to the district hospitals using refrigerated trucks, while the military helped get vaccines to more remote districts using helicopters. “On the first day, all vaccines were in the district according to the number the district had reported needed, because the preparation was there before,” said Binagwaho.
Tackling vaccine hesitancy
Africans view COVID-19 vaccines as less safe than other vaccines
In an Africa CDC survey, most respondents viewed COVID-19 vaccines as less safe than those for other diseases. Health experts are calling for continuous surveillance as countries roll out vaccines.
Another challenge has been health care worker’s attitude towards vaccines, said Dr. John Nkengasong, director at the Africa Centers for Disease Control and Prevention. “It’s very variable across the continent and it’s not making it easy for vaccine uptake,” he said, adding that tackling hesitancy remains a key priority area to invest in.
Misinformation and a lack of trust is at the core. “Concerns regarding the safety and efficacy of COVID-19 vaccines continue to circulate on social media, driven by misinformation and disinformation about COVID-19 and vaccines. A lack of trust is linked to vaccine hesitancy,” wrote WHO’s Dr. Atuhebwe in an email to Devex.
A strategy used to tackle vaccine hesitancy amongst health care workers in Kenya had the nurse in charge of each county publicly take the vaccine to encourage other staff working under them to also take it, said Akhwale.
Printing articles to share with others is a breach of our terms and conditions and copyright policy. Please use the sharing options on the left side of the article. Devex Pro subscribers may share up to 10 articles per month using the Pro share tool ( ).
from WordPress https://ift.tt/3uQkdKY
via IFTTT

No comments:
Post a Comment