In a remote South African village, set in windswept hills not far from the Indian Ocean, Nolindele Mdibanto fears she will never get the Covid-19 vaccine.
The nearest government clinic to Nqileni, deep in the rural Eastern Cape, lies several miles beyond a river and over hilly terrain. Despite daily hikes to fetch firewood and water for her thatched one-room home, the prospect of a long trek unnerves the Xhosa elder.
“Now I’m too old, and it’s not easy to walk,” said Mdibanto, who is in her eighties and says she successfully “kicked away” a mild Covid-19 infection during a recent outbreak. “They say it’s coming, but it will take a long time, or it will never come.”
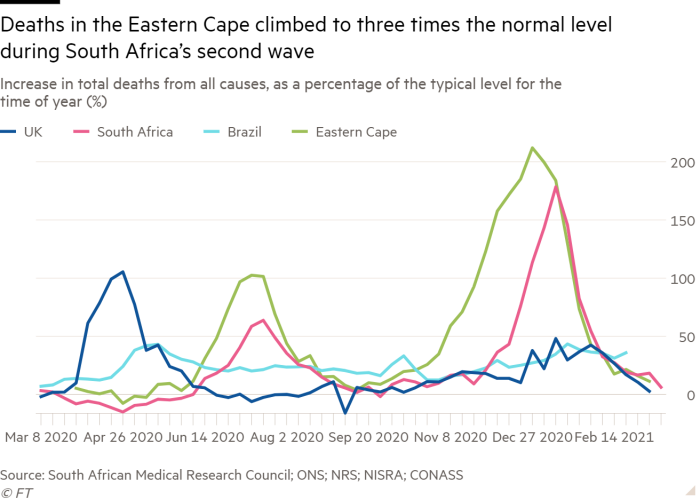
The Eastern Cape, one of South Africa’s most deprived provinces, is one of the regions in the world hardest hit by the pandemic. It is the first place the more infectious 501.V2 variant was seen and “excess” deaths above statistical norms over the past year are estimated to be about 32,000, equivalent to nearly one in 200 of its 6.7m population.
The figures reflect mismanaged hospitals, shortages of supplies such as oxygen and poor infrastructure, say experts. These issues will also test the limits of South Africa’s vaccine rollout, which began in February and will kick off an ambitious nationwide phase for the elderly, vulnerable and other high-risk groups within months.
How the vaccination campaign goes in places such as Nqileni will have an impact not only in South Africa — which with 52,000 official deaths is the worst hit on the African continent — but for vaccination drives everywhere. As rich countries press ahead with their immunisation efforts, what will be the biggest vaccination campaign in history is only just beginning in the developing world.
As has now become a mantra, Covid-19 will not be contained anywhere until it is suppressed everywhere, a reality brought home by the rapid spread of variants such as 501.V2, some of which are more resistant to current vaccines. And while South Africa and other developing countries are well versed in mass childhood vaccination campaigns, they have far less experience in getting vaccines to adults like Mdibanto.
While officially the old and sick of Nqileni and nearby villages are in line for jabs “it is extremely worrying that we could be forgotten”, said Lynne Wilkinson, acting director of the Bulungula Incubator, a local non-profit.

So far, South Africa has vaccinated just over one in 10 of an initial phase of 1.25m frontline health workers, in part because of limited supplies. The second stage, targeting about 16m out of a population of 58m, is due to begin in April.
The country’s vaccination planning was dealt a blow last month when it suspended an initial rollout of the Oxford/AstraZeneca vaccine after a preliminary study found it was not effective against milder illness with the 501.V2 variant.
It was replaced with Johnson & Johnson’s single-dose jab, but there have been limited supplies so far. Larger deliveries of the J&J and BioNTech/Pfizer vaccines are expected to underpin the second phase. Rollout must accelerate to at least 150,000 to 250,000 doses a day to protect a large portion of the population by the end of the year, business leaders have said.
“It’s going to be a tough one,” said Russell Rensburg, director of South Africa’s Rural Health Advocacy Project.
There will be difficult questions over access in both cities, where major outbreaks have been centred, and rural areas, such as the Eastern Cape. “If you’re going to go rural, do everyone when you’re there. We shouldn’t expect people to go to [central vaccination sites], but go on vaccination drives,” said Rensburg.
J&J’s one-shot vaccine, which is stored at normal fridge temperatures, “helps a lot” with these problems, Rensburg added. Because it needs colder storage and patience for two doses, “in practice, the Pfizer vaccine is better suited to GP practices and urban areas”.
Difficulty in vaccinating older people
Nqileni, which was relatively unscathed during the second wave, is an hour or more car journey down bone-shaking gravel from Mthatha, the nearest big city, and 40km from a hospital. Not even public ambulances brave the bad roads.
Nor is its situation unique. In January, health officials said that nearly 3,000 communities in the province were more than 5km from the nearest health facility and that schools and other sites were being considered for vaccinations.
If the government health clinic over the river is the only local place for distributing vaccines in the months to come, “old people, it’s going to be hard for them”, said Nosomeleze Sontundu, a community health worker who is still waiting for her own jab. “The road to the clinic is for the strong and healthy. It is not for the old and sick.”
It would be just about possible to arrange transport for nearly two dozen health workers across four villages to receive jabs at distant clinics or hospitals, Wilkinson said. “When we start moving to the old people, that is completely not feasible.”
So urgent is the problem that the Bulungula Incubator is even installing a solar system at a small “health point” sub-clinic it runs in Nqileni to power a fridge for vaccines. Doses “would be stored at the health point but ideally, they would go into the villages”, Wilkinson said.

Vaccines are also key for life in the community to properly restart. This year the villages’ first local high school, which opened its doors in 2019, is putting through its first-ever cohort for South Africa’s high-school leaving qualification.
The first graduates from Bulungula College would be a “historical moment for everybody” because it promises to break a cycle of high dropout rates and migration out of the area for work, said Nosintu Gwebindlala, chair of the Bulungula Incubator and the community’s presiding traditional leader. Students are already attending Saturday and evening classes to catch up after nationwide school closures last year. Without vaccines, studies could be disrupted more.
In tandem with posters and WhatsApp messages, a community radio station run by the incubator is assuring listeners that vaccines will arrive and dispelling myths, since the last adult inoculations in the region date back to polio.
Gwebindlala wants the government to be more proactive on vaccines. “When it’s election time, they do have resources, they do go door to door,” she said. “It would be nice if they can use the same energy they have when they are campaigning.”


Meanwhile, as a traditional chief mediating between her community and a distant state, Gwebindlala is grappling with an even more fundamental problem. She is trying to register people for vaccination but some of Nquileni’s population “do not have IDs”, she said. “It’s my worry every day. I don’t sleep.”
Mdibanto is one such elder who does not know her exact age, although a record book kept in her traditional rondavel home indicated she was born some time in 1939. The government might be promising vaccines, but, “like the ambulances”, she said, “they say they’re coming, but we don’t see them”.
from WordPress https://ift.tt/3rgveDR
via IFTTT

No comments:
Post a Comment